Sleep Apnea in Singapore: Your Guide to Better Sleep
What is Sleep Apnea?
Sleep apnea is a serious sleep disorder that affects breathing during sleep. Characterised by pauses in breathing, it leads to oxygen deprivation and, if left untreated, can result in various health problems. This condition manifests in several forms, including Obstructive Sleep Apnea (OSA), Central Sleep Apnea (CSA), and Treatment-Emergent Central Sleep Apnea (TECSA).
Common symptoms of sleep apnea include loud snoring and excessive daytime sleepiness. Read on to learn more about what the condition entails, how it’s diagnosed, and how you can help yourself or your loved ones manage this challenging condition.
How Common is Sleep Apnea?
In Singapore, a Jurong Health Services study has revealed a concerning prevalence of sleep apnea. It found that one in three Singaporeans suffers from moderate to severe sleep apnea, and one in ten from severe sleep apnea. Despite its commonality, the condition remains largely under-diagnosed, severe cases being previously undiagnosed. This highlights the need for increased awareness and diagnosis to address potential health risks associated with untreated sleep apnea.

Types of Sleep Apnea
Sleep apnea is a common sleep disorder characterised by pauses in breathing or shallow breaths during sleep. It primarily falls into two categories: Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA). Each type has distinct causes and characteristics, affecting the respiratory pattern differently.
Obstructive Sleep Apnea (OSA)
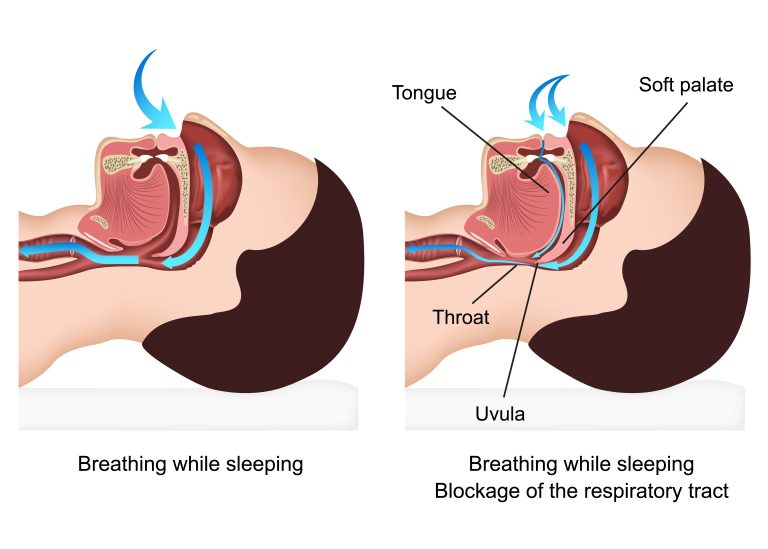
Obstructive Sleep Apnea is the most common form of sleep apnea. It occurs when the muscles in the throat relax excessively during sleep, leading to a blocked airway. In many cases of OSA, the soft tissues of the throat, such as the uvula and soft palate, relax excessively during sleep, obstructing the airway and leading to apnea events.
Reduced airflow causes repeated breathing pauses, known as apneas, which can reduce oxygen flow to vital organs and disrupt sleep. Common symptoms include loud snoring, gasping for air during sleep, and feeling tired after a full night’s rest. OSA is often associated with factors like obesity, anatomic structure of the jaw and neck, and lifestyle habits.
Apnea-Hypopnea Index (AHI) in Sleep Apnea Diagnosis
The Apnea-Hypopnea Index (AHI) is a critical measure used by healthcare professionals to diagnose and assess the severity of sleep apnea. It is calculated based on the number of apnea (complete pauses in breathing) and hypopnea (partial reductions in breathing) episodes that occur per hour of sleep.
- Mild Sleep Apnea: An AHI of 5 to 15 events per hour is typically considered mild sleep apnea. In this stage, patients might experience some sleep disturbances and daytime fatigue, but the overall impact on health is less severe.
- Moderate Sleep Apnea: An AHI between 15 and 30 signifies moderate sleep apnea. This level is often associated with more noticeable symptoms such as louder snoring, frequent awakenings, and significant daytime drowsiness, which may start impacting daily life.
- Severe Sleep Apnea: An AHI over 30 is indicative of severe sleep apnea. This stage poses a higher risk of health complications, including cardiovascular issues, cognitive impairment, and severe daytime fatigue that can significantly impair an individual’s quality of life.
Understanding one’s AHI score is crucial for determining the appropriate treatment approach. For instance, mild cases might be managed with lifestyle changes, whereas moderate to severe cases often require more intensive treatments like CPAP therapy or even surgery.
Central Sleep Apnea (CSA)
Central Sleep Apnea is less common and involves the central nervous system, often leading to potentially high diastolic blood pressure.
In CSA, the brain fails to send proper signals to the muscles that control breathing. This leads to regular interruptions in breathing patterns, even though there are no blockages in the airway. CSA often involves abnormal breathing patterns, such as Cheyne-Stokes respiration, characterised by rhythmic variations in breathing depth and rate.
Unlike OSA, CSA is often linked to underlying health conditions like heart failure or stroke. Symptoms may include shortness of breath, insomnia, or chronic fatigue. Treatment typically focuses on the underlying condition as well as improving breathing patterns during sleep.
Treatment-Emergent Central Sleep Apnea (TECSA)
Treatment-emergent central sleep apnea (TECSA), also known as complex sleep apnea syndrome, is a type of sleep apnea that develops in some people during treatment for obstructive sleep apnea (OSA), typically when using Continuous Positive Airway Pressure (CPAP) therapy. In TECSA, the airway remains open, but the brain doesn’t send the necessary signals to breathe regularly. This condition is observed after the obstructive events of OSA have been resolved or reduced, and it can be temporary. TECSA may require adjustments in treatment, and it often resolves over time as the body adapts to the therapy.
What Causes Sleep Apnea?
In general, the factors below influence your likelihood of contracting sleep apnea and experiencing breathing difficulties at night, or even in the day.
The likelihood of developing sleep apnea increases with age.
Excess weight or obesity significantly raises the risk of sleep apnea.
Higher prevalence is observed in Black, Hispanic, and Asian populations.
Higher altitudes can lead to the occurrence of central apneas.
Sleep Cycle
Understanding sleep apnea involves knowing about the human sleep cycle, which consists of several stages:
- Stage 1: Light sleep, marking the start of sleep and comprising about 5% of total sleep time.
- Stage 2: A deeper sleep state, making up roughly 45-50% of sleep, increasing with age.
- Stage 3: The deepest sleep stage, accounting for about 25% of sleep, decreasing with age. Waking from this stage often leads to sleep inertia, a state of mental grogginess. Sleepwalking and sleeptalking typically occur in this stage.
- REM Sleep: Characterised by rapid eye movement and dreaming.
The sleep cycle starts in Stage 1 and moves through these stages, cycling between Stages 2 and 3 before entering REM sleep. Each cycle lasts about 90 to 110 minutes, with several cycles occurring each night.
The causes of sleep apnea can be categorised into those more commonly associated with Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA).
Obstructive Sleep Apnea (OSA):
- Age: Increases risk, especially in middle-aged and older adults.
- Gender: More common in men or those assigned male at birth.
- Body Weight: Higher BMI linked to increased OSA risk.
- Neck Circumference: Larger necks may narrow the airway.
- Smoking: Raises the likelihood of developing OSA.
- Nasal Congestion: Can contribute to OSA.
- Hormone Abnormalities: May cause tissue swelling near the airway.
- Anatomical Features: Large tongue, short lower jaw can be factors.
- Sleeping Position: Back sleeping can worsen OSA.
- Family History: Genetic predisposition related to head and neck anatomy.
Central Sleep Apnea (CSA):
- Age: Higher risk in individuals over 65.
- Gender: More common in men or those assigned male at birth.
- Medical Conditions: Heart or kidney failure, stroke increase risk.
- High Altitude: Decreased oxygen availability can lead to CSA.
- Medication Use: Chronic opioid use and some prescriptions linked to higher CSA risk.
Treatment Emergent Central Sleep Apnea:
- CPAP Therapy: Using a CPAP machine for obstructive sleep apnea treatment can sometimes lead to central apneas.
- Individual Sensitivity: Some people may be more susceptible to developing central apneas during CPAP therapy due to their unique sensitivities.
- Adaptive Servo-Ventilation (ASV): ASV therapy, used to treat sleep apnea, may paradoxically trigger central apneas in certain cases.
- Complex Sleep Apnea Syndrome: Some individuals with OSA can transition to a condition called Complex Sleep Apnea Syndrome, which combines obstructive and central apneas during treatment.
How Does Sleep Apnea Affect My Body?
In obstructive sleep apnea (OSA), the cessation of breathing leads to increased carbon dioxide levels in the blood. This can cause headaches and daytime fatigue due to CO2 buildup. Additionally, conditions like chronic obstructive pulmonary disease (COPD) and asthma may exacerbate or coexist with sleep apnea, complicating its management.
Sleep Apnea Symptoms
Signs of sleep apnea in adults:
- Experiencing morning headaches.
- Feeling unusually restless and experiencing night sweats.
- Encountering memory loss and concentration difficulties.
- Noticing changes in mood, such as depression or anxiety.
- Waking up with a sensation of choking or shortness of breath.
- Having insomnia.
- Observing pauses in breathing while asleep.
- Experiencing daytime drowsiness, affecting activities like driving or working.
- Dealing with sexual dysfunction.
- Waking up tired, despite a full night’s sleep.
- Snoring (not always present in every case).
- Nightly awakenings, often without recollection.
- Exhibiting unusual breathing patterns, like Cheyne-Stokes breathing in central sleep apnea.

Presentation in Men vs Women
| Symptom | Men | Women |
| Snoring | Loud and persistent | Less obvious, intermittent |
| Daytime Fatigue | Often attributed to work stress or ageing | Often mistaken for stress or hormonal changes |
| Breathing Interruptions | Noticeable, with gasping or choking | Subtler, may not be noticed |
| Mood Changes | Less commonly reported | More commonly reported (depression, anxiety) |
| Nighttime Awakenings | Frequent, with gasping or choking | Less frequent or noticeable |
| Health Risks | Higher risk of heart disease, stroke | Increased risk of hypertension, heart issues |
Signs of sleep apnea in children:
- Showing hyperactivity, focus difficulties, and performance issues in school, similar to ADHD.
- Exhibiting loud snoring.
- Experiencing bedwetting.
- Displaying frequent arm or leg movements during sleep.
- Sleeping in odd positions or with an extended neck.
- Suffering from reflux or night sweats.
Who is a Good Candidate For Sleep Apnea Treatment?

Appropriate care for sleep apnea involves a personalised approach, taking into account the patient’s overall health, the severity of the apnea, and their response to initial treatments.
Ideal Candidates:
✔ Persistent Symptoms: Individuals experiencing ongoing symptoms of sleep apnea despite trying non-medical therapies.
✔ Moderate to Severe Apnea: Diagnosed with moderate to severe obstructive or central sleep apnea.
✔ Comorbid Conditions: Individuals with other health conditions like heart disease or diabetes that could be worsened by sleep apnea.
Less Ideal Candidates:
✖ Mild Sleep Apnea: Those with very mild symptoms might not require intensive treatment.
✖ Lifestyle-related Causes: Individuals whose apnea can be resolved through lifestyle changes like weight loss.
✖ Non-compliant Patients: Those unwilling or unable to adhere to treatment regimens, especially CPAP.
Sleep Apnea Diagnosis
Sleep apnea is typically diagnosed using specialised tests such as polysomnography and home sleep apnea testing. Polysomnography, conducted in a sleep lab, is considered the most comprehensive diagnostic tool. It measures various body functions during sleep to give detailed insights necessary for personalised treatment.
Clinical decision support systems are increasingly used to help healthcare providers choose the most appropriate diagnostic tests and treatments for sleep apnea patients. For expert diagnosis and treatment of sleep apnea, consider consulting with our professionals at Nuffield ENT.
Polysomnography

This in-lab sleep study is considered the most comprehensive tool for diagnosing sleep apnea. During polysomnography:
- Patients spend a night at a sleep centre, where they are monitored throughout their sleep.
- Various physiological parameters are recorded, including brain waves (to assess different sleep stages), eye movements, muscle activity, heart rate, respiratory effort, airflow, and blood oxygen levels.
- This extensive data collection helps in identifying the type and severity of sleep apnea, as well as other sleep disorders that might coexist.
- PSG is particularly beneficial for patients with suspected complex sleep apnea or those with other sleep-related health issues.
Home Sleep Apnea Testing

This test offers a more convenient but less comprehensive alternative to PSG.
- HSAT involves using a portable monitoring device at home while sleeping.
- The device typically records breathing patterns, blood oxygen levels, heart rate, and sometimes air flow.
- While not as detailed as PSG, HSAT can be sufficient for diagnosing obstructive sleep apnea in uncomplicated cases.
- HSAT is particularly useful for patients who cannot easily travel to a sleep centre, or for initial screening when sleep apnea is strongly suspected.
Both tests are crucial for ensuring an accurate diagnosis and effective treatment plan. The choice between PSG and HSAT depends on the individual’s specific circumstances, symptoms, and potential co-existing conditions. After diagnosis, a healthcare provider will discuss the most suitable treatment options based on the test results and overall health status of the patient.
Concluding this diagnostic journey, it’s also important to highlight the initial steps of assessing medical history and conducting a physical exam. Your doctor will review your symptoms, family history of sleep disorders, and any complications indicative of undiagnosed sleep apnea. During the physical examination, they will assess various physical factors like obesity, airway structure, and neurological signs that could contribute to sleep apnea. This comprehensive approach ensures a thorough understanding and effective management of the condition.
Sleep Apnea Treatment Singapore
Treatments for OSA include:
- Continuous Positive Airway Pressure (CPAP) therapy: This therapy uses a machine to deliver a steady stream of air through a mask, keeping the airway open during sleep. It’s commonly used for sleep apnea.
- Automatic Positive Airway Pressure (APAP) Therapy: Similar to CPAP, but the machine automatically adjusts the air pressure level throughout the night based on your breathing patterns.
- Other Airway Pressure Devices: These are variations of CPAP and APAP machines, designed to cater to specific needs, like different pressure levels or humidification.
- Oral Appliances: These are custom-fitted devices, similar to mouthguards, that help keep the airway open by positioning the jaw or tongue during sleep.
- Supplemental Oxygen: This involves using extra oxygen, usually through a mask or nasal tube, to ensure the body gets enough oxygen during sleep, especially in cases of severe sleep apnea.
- Adaptive Servo-Ventilation (ASV): This advanced therapy uses a machine that adjusts air pressure and flow based on your breathing patterns, specifically designed for complex or central sleep apnea.
- Surgery Options: These can include:
- Tissue Removal: Removing excess tissue from the throat to widen the airway.
- Jaw Repositioning: Moving the jaw forward to increase the size of the upper airway.
- Implants: Placing plastic rods in the soft palate to keep the airway open.
- Nerve Stimulation: Stimulating nerves to keep the airway muscles open.
- Tracheostomy: Creating a new air passage in the neck for severe cases.
For CSA, treatments primarily involve:
- Adaptive Servo-Ventilation (ASV): Tailored for CSA, it adjusts pressure based on breathing patterns to normalise breathing.
- Bilevel Positive Airway Pressure (BiPAP): Provides two levels of air pressure, higher during inhalation and lower during exhalation, suitable for CSA and other respiratory conditions.
- Supplemental Oxygen: To ensure adequate oxygen levels during sleep in CSA patients.
- Medications: Which can help regulate breathing patterns in some cases of CSA.
In some cases, when other treatments like CPAP therapy or oral appliances are not effective, individuals with sleep apnea may consider sleep apnea surgery. Surgical procedures can include the removal of excess tissue in the throat, jaw repositioning, implants, nerve stimulation, or tracheostomy.
Sleep Apnea Complications
Complications from Obstructive Sleep Apnea (OSA):
| Complication | Impact of OSA |
| Daytime Tiredness & Mood Disorders | Leads to severe fatigue, mood swings, and heightened risk of mood disorders due to disrupted sleep. |
| Cardiovascular Problems | Increases risks of hypertension, heart attacks, and heart failure. Heart attack risk is 2 to 3 times higher. |
| Stroke | Nearly 70% of stroke victims also have OSA. |
| Type 2 Diabetes & Metabolic Syndrome | Elevates the chance of developing these conditions. |
| Surgery Complications | Increases risks related to anaesthesia and recovery. |
| Liver Complications | Linked to nonalcoholic fatty liver disease. |
| Impact on Partners’ Sleep | Causes sleep disruption for partners due to loud snoring. |
| Memory Loss | Can lead to cognitive impairments including memory issues. |
| Depression | Raises the likelihood of developing depression. |
| Risk of Accidents | 7 times more likely to be involved in motor vehicle accidents; increased risk of work-related accidents. |
Complications from Central Sleep Apnea (CSA):
| Complication | Impact of CSA |
| Prevalence in Adults Over 40 | About 0.9% of adults over 40 in the US are affected by CSA. |
| Association with Heart Failure | Approximately 40% of individuals with Congestive Heart Failure also suffer from CSA. |
| Association with Parkinson’s Disease | Up to 40% of individuals with Parkinson’s Disease may experience CSA. |
| Treatment Challenges | Treatment includes addressing the underlying cause, and various PAP therapies like CPAP and ASV, but finding the optimal therapeutic strategy can be complex. |
| Daytime Drowsiness and Concentration Issues | CSA can lead to fragmented sleep, resulting in daytime drowsiness, attention deficits, and an increased risk of errors and accidents. |
Untreated sleep apnea can negatively influence various health outcomes, including cognitive function, workplace performance, and even emotional well-being.
Travelling With Sleep Apnea
Before You Travel:
✅ Travel-Sized CPAP Machine: Consider a compact CPAP machine for easier travel.
✅ Check Voltage Compatibility: Ensure your CPAP machine works with local voltage.
✅ Power Adapter: Pack a versatile power adapter for different outlets.
✅ Portable Battery: Carry a charged portable battery for backup power.
During Your Trip:
✅ Accommodation Planning: Confirm if your lodging offers power sources for your CPAP.
✅ Doctor’s Note: Carry a letter from your healthcare provider explaining your condition.
✅ Cleaning Supplies: Bring small cleaning supplies for your CPAP mask and machine.
✅ Travel-Size Humidifier: Use a compact humidifier to combat dryness.
✅ CPAP Travel Bag: Invest in a specialised bag for CPAP equipment.
✅ Noise-Canceling Gear: Block out noise with earplugs or headphones.
Sleep Comfortably:
✅ Travel Pillow: Opt for a CPAP-friendly travel pillow.
✅ Stay Hydrated: Drink plenty of water, especially during flights.
✅ Adjust Sleep Schedule: Gradually shift your sleep schedule to minimise jet lag.
✅ Local Healthcare Services: Know local healthcare options for emergencies.
✅ Backup Plan: Prepare for machine malfunctions or loss with a backup solution.
With these condensed travel tips, you can ensure a comfortable and uninterrupted sleep experience while travelling. Safe travels!
Tips on Living With Sleep Apnea
To effectively manage sleep apnea and promote better health outcomes, consider the following lifestyle changes:
- Maintain a Healthy Weight: This is crucial for reducing symptoms.
- Regular Physical Activity: Engage in exercises to improve symptoms and manage weight.
- Good Sleep Hygiene: Ensure your bedroom is dark and quiet, and maintain a consistent sleep schedule.
- Side Sleeping: Sleep on your side to reduce symptoms, using tactics like the tennis ball method or a special pillow.
- Avoid Harmful Substances: Refrain from smoking, excessive alcohol, and unadvised sleeping pills, as these can worsen sleep apnea.
- Device Maintenance: Keep any Positive Airway Pressure (PAP) or oral devices clean and functional.
- Be Cautious of Daytime Sleepiness: Avoid activities like driving when drowsy.
- Regular Exercise and Relaxation: Incorporate exercises and relaxation techniques like yoga for overall health improvement.
- Inform Healthcare Providers: Always tell new healthcare providers about your sleep apnea, especially when considering new medications or procedures.
- Regular Doctor Visits: Keep in constant touch with your doctor or sleep specialist for effective condition management.

Conclusion
Recognising and addressing sleep apnea is pivotal for maintaining good health and quality of life. This disorder, affecting a significant portion of the population, requires attention and care. At Nuffield ENT, we are dedicated to providing expert diagnosis and tailored treatments for those suffering from sleep apnea. Embrace the path to improved sleep and overall wellness by reaching out to our team at Nuffield ENT any time. Let us guide you towards a restful night and a healthier tomorrow.
FAQ Section
1. Can Sleep Apnea Kill You?
Yes, sleep apnea is a serious medical condition that, if left untreated, can lead to significant health issues and even death. Individuals with untreated sleep apnea are at an increased risk of heart disease, high blood pressure, stroke, and type 2 diabetes. It can also lead to or worsen heart failure. Additionally, sleep apnea can contribute to chronic fatigue, which increases the risk of workplace or driving accidents due to drowsiness.
2. Is Sleep Apnea Genetic or Hereditary?
Sleep apnea can have a hereditary component. Genetics can influence factors like the structure of the jaw and airway, which are associated with obstructive sleep apnea. Additionally, family history of sleep apnea or related conditions can increase the likelihood of developing it. However, environmental factors and lifestyle choices also play significant roles in its onset.
3. What is the Life Expectancy of a Person with Sleep Apnea?
Untreated sleep apnea can negatively impact life expectancy due to its association with several severe health conditions. However, effective treatment can substantially reduce these risks. Early diagnosis and consistent treatment can improve overall health and potentially normalise life expectancy.
4. At What Age is Sleep Apnea Most Common?
Sleep apnea can occur at any age but is most commonly diagnosed in adults between 40 and 60 years. However, risk factors like obesity, family history, and certain health conditions can influence its onset at different ages.
5. How Can I Reduce My Risk or Prevent Sleep Apnea?
To reduce the risk or prevent sleep apnea:
- Maintain a healthy weight.
- Exercise regularly.
- Avoid alcohol and sedatives.
- Stop smoking.
- Sleep on your side.
- Keep nasal passages open at night.
- Treat allergies or nasal issues.
6. How to Cure Sleep Apnea?
Unfortunately, there is no cure for sleep apnea: it’s a chronic condition that has to be managed carefully. Lifestyle changes, such as weight loss and exercise, can fully resolve symptoms, particularly those caused by obesity. However, other forms, especially severe cases, may require ongoing management using CPAP machines, oral appliances, or surgery. The goal of treatment is to manage symptoms and reduce the risk of complications.
7. What’s the Difference Between Snoring and Sleep Apnea?
Snoring is a loud breathing sound during sleep, often harmless. Sleep apnea involves repeated breathing interruptions during sleep, leading to health risks. Not all who snore have sleep apnea, but snoring is a common symptom of the condition.
8. What is the Best Position to Sleep if You Have Sleep Apnea?
Sleeping on the side is generally considered the best position for those with sleep apnea. It helps keep the airways open and reduces the likelihood of the tongue and soft tissues obstructing the airway, which is more common when lying on the back.
9. What Can or Can’t I Eat or Drink with Sleep Apnea?
Diet plays a significant role in managing sleep apnea. It’s advisable to avoid heavy meals, caffeine, and alcohol before bedtime as they can interfere with the sleep cycle and relax throat muscles, exacerbating the apnea. A balanced diet that promotes a healthy weight is crucial; obesity is a major risk factor for obstructive sleep apnea. Weight loss can reduce the severity of symptoms in some individuals.
10. Can I Drive if I Have Sleep Apnea?
You can drive with sleep apnea, but it’s crucial to manage the condition effectively. Untreated sleep apnea can lead to severe daytime drowsiness, increasing the risk of accidents. If you’re receiving treatment and no longer experience significant daytime sleepiness, driving may be safe. However, it’s important to consult with your doctor and adhere strictly to your treatment plan to ensure your safety and that of others on the road. With consistent treatment, you’ll be able to drive better.
11. My Child Has Sleep Apnea. How Can I Better Support Him/Her?
To support a child with sleep apnea, ensure consistent follow-up with a pediatric sleep specialist. Create a comfortable sleep environment, encourage healthy weight and diet, and help them adhere to any prescribed treatments, like CPAP if needed. Be attentive to their emotional well-being, as sleep apnea can affect mood and school performance. Most importantly, maintain open communication with your child and their healthcare providers to effectively manage their condition.
Sleep Apnea Myths & Facts
Myth #1: Sleep apnea only affects older, overweight men.
Fact: Sleep apnea can affect people of any age, including women and children. While it is more common in older men, other factors such as family history, nasal congestion, and anatomical differences can also contribute to the risk.
Myth #2: Snoring is always a sign of sleep apnea.
Fact: Not everyone who snores has sleep apnea, though snoring is a common symptom. There are many other factors that contribute to snoring. However, if snoring is accompanied by choking or gasping for air, it may indicate sleep apnea.
Myth #3: Sleep apnea is not a serious condition.
Fact: Sleep apnea is a serious medical condition that can lead to significant health complications if left untreated. It increases the risk of high blood pressure, heart disease, stroke, diabetes, and depression.
Myth #4: CPAP is the only treatment for sleep apnea.
Fact: While CPAP (Continuous Positive Airway Pressure) is one of the most common and effective treatments for sleep apnea, there are other treatments available. These include oral appliances, lifestyle changes, positional therapy, and surgery, depending on the severity and type of sleep apnea.
Myth #5: Sleep apnea treatments are cumbersome and uncomfortable.
Fact: Many modern sleep apnea treatments are designed for comfort and ease of use. CPAP machines have become quieter and more comfortable over the years. Additionally, alternatives like oral appliances are custom-made for the patient, ensuring a better fit and comfort.
Medical References
Dredla, B. K., & Castillo, P. R. (2019). Cardiovascular consequences of obstructive sleep apnea. Current Cardiology Reports, 21(11). https://doi.org/10.1007/s11886-019-1228-3
Gottlieb, D. J., & Punjabi, N. M. (2020). Diagnosis and management of obstructive sleep apnea. JAMA, 323(14), 1389. https://doi.org/10.1001/jama.2020.3514
Lin, J., & Suurna, M. V. (2018). Sleep Apnea and Sleep-Disordered Breathing. Otolaryngologic Clinics of North America, 51(4), 827–833. https://doi.org/10.1016/j.otc.2018.03.009
