Sleep Apnea Treatment in Singapore:
Explore Your Options
Sleep apnea is a condition where your breathing stops and starts repeatedly during sleep, leading to various symptoms that can affect anyone. In this easy-to-understand guide, we’ll explore a range of treatments that can help, from simple lifestyle changes to devices like CPAP machines that keep your airways open, and even surgery for more severe cases. So, are you ready to make a change? Let’s get started.
Sleep Apnea Treatment: Diagnosis
Polysomnography (PSG) is an in-lab sleep study considered the gold standard for diagnosing sleep apnea, providing extensive data including brain waves and muscle activity. Home Sleep Apnea Testing (HSAT) is a convenient at-home alternative, suitable for initial screening, but with less comprehensive data compared to PSG.
| Diagnosis Method | Polysomnography (PSG) | Home Sleep Apnea Testing (HSAT) |
| Description | In-lab sleep study is considered the most comprehensive diagnostic tool. | Convenient at-home test offering a simpler diagnostic approach. |
| Pros | Comprehensive Data: Extensive monitoring including brain waves, muscle activity, airflow, etc. Identifies Coexisting Conditions: Reveals other sleep disorders. Best for Complex Cases: Ideal for patients with complex sleep apnea or additional sleep-related health concerns. | Convenience: Can be done at home. Essential Data: Records critical data like breathing patterns and blood oxygen levels. Great for Initial Screening: Useful for those unable to visit a sleep centre or as a first step when sleep apnea is suspected. |
| Cons | Inconvenience: Requires an overnight stay at a sleep centre. Time-Intensive: May involve a waiting period for availability. | Limited Data: Less comprehensive than PSG, potentially missing nuanced details. Accuracy Concerns: Self-administration can lead to potential errors in data collection. |
Types of Sleep Apnea and Their Treatments
In Singapore, renowned institutions like the National University Hospital (NUH) Sleep Disorder Clinic offer comprehensive sleep apnea management programs. With a focus on personalised care, these clinics utilise a multidisciplinary approach, integrating the latest research and technologies to ensure optimal treatment outcomes. At Nuffield, we’re committed to matching you with the appropriate treatment option. Feel free to reach out to us at any time.
Treatment for Obstructive Sleep Apnea
Mild Obstructive Sleep Apnea Treatment
Fundamentally, mild OSA management involves lifestyle modifications, which will be elaborated on in the following sections.
For some patients, particularly those with mild to moderate OSA or who snore, a Mandibular Advancement Appliance (MAD) may be an effective treatment. MAD works by advancing the lower jaw and its contents (including the tongue), thereby increasing the tension in the muscles responsible for keeping the upper airway open during sleep. Not only does this reduce the severity of apnea events, it also improves overall sleep quality.
Severe Obstructive Sleep Apnea Treatment
Severe OSA may necessitate CPAP therapy or advanced surgical procedures. Surgical options aim to enlarge the airway and may include tissue removal, jaw repositioning, or newer treatments like hypoglossal nerve stimulation. Another effective surgical option is Somnoplasty, which uses radiofrequency energy to trim excess tissue in the upper airway, providing a minimally invasive solution to reduce tissue obstruction and improve airflow during sleep.
Central Sleep Apnea Treatment
Central Sleep Apnea (CSA) treatments include addressing underlying conditions, using oxygen supplementation, or Positive Airway Pressure machines. Adaptive Servo-Ventilation (ASV) is effective, adjusting airflow in response to breathing patterns, ensuring stable breathing during sleep.
Complex Sleep Apnea Treatment
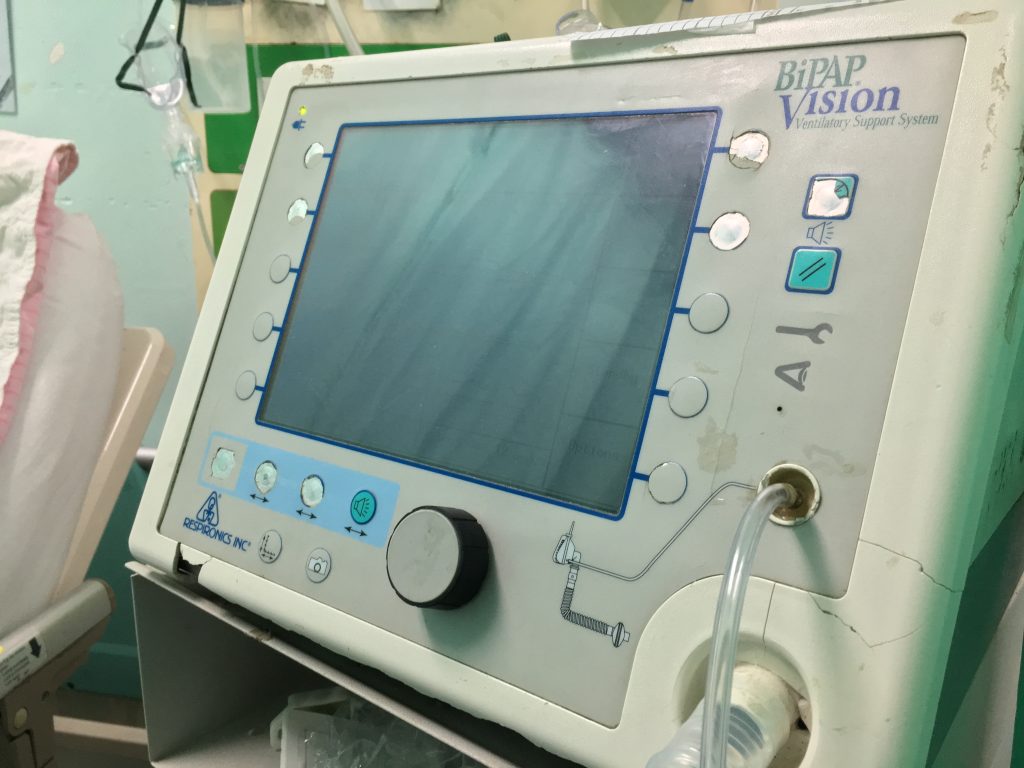
Complex Sleep Apnea, a combination of OSA and CSA, is challenging to treat. Management often starts with CPAP therapy. If ineffective, treatments like ASV, which customises air pressure based on real-time breathing patterns, or Bilevel Positive Airway Pressure (BiPAP) machines, offering varied inhalation and exhalation pressures, are considered.
Non-Invasive Sleep Apnea Treatment Options
These treatments are minimally invasive and can help relieve sleep apnea symptoms. For personalised mask fittings, proper education, and continuous support, our team at Nuffield are always ready to assist you.

1. CPAP (Continuous Positive Airway Pressure) Machines
- How it Works: The CPAP machine delivers a continuous stream of air through a mask that covers the nose, mouth, or both. This consistent airflow creates enough pressure to keep the airways open, preventing the breathing interruptions characteristic of sleep apnea.
- Pressure CPAP: Machines can be set at different pressure levels, tailored to the patient’s needs. Higher pressures may be necessary for severe cases of obstructive sleep apnea, while lower pressures might be sufficient for mild to moderate conditions.
- Benefits for the User: Users often experience a significant reduction in sleep apnea symptoms, like snoring and daytime fatigue, leading to better overall sleep quality and health. The enhanced comfort and usability of the latest CPAP models also mean patients are more likely to use them consistently, which is crucial for effective treatment.
2. BiPAP (Bilevel Positive Airway Pressure) Machine
- How it Works: BiPAP machines deliver two levels of air pressure: a higher pressure when you inhale and a lower pressure when you exhale. This dual-setting approach helps patients who struggle with the continuous pressure of a CPAP machine by making it easier to breathe out against the incoming airflow.
- Benefits for the User:
- Is comfortable due to the lower expiratory pressure, making it more tolerable for users and increasing the likelihood of adherence to therapy. This can lead to better compliance, improved sleep quality, and reduced daytime fatigue.
- Additionally, for patients with other respiratory conditions such as COPD (Chronic Obstructive Pulmonary Disease), the BiPAP can assist with breathing and improve oxygenation, enhancing overall treatment efficacy. Users may find that the BiPAP’s ability to adjust to their breathing makes it easier to use, promoting consistent use and leading to more restful nights.
3. Adaptive Servo-Ventilation (ASV)
- How it Works: ASV machines adapt to the user’s breathing pattern. They provide more air when needed and less when not, ensuring a more natural breathing rhythm during sleep. This adaptability makes ASV particularly effective for patients whose breathing patterns vary significantly throughout the night.
- Benefits for the User: ASV can significantly improve sleep quality for patients with complex and central sleep apnea conditions. Users often report better sleep and fewer awakenings during the night.

4. Oral Devices
- How it Works: Dentists custom-fit these devices, which are designed to keep the airway open while you sleep. The most common types are mandibular repositioning mouthpieces, which push the lower jaw forward and down slightly to prevent airway obstruction, and tongue-retaining devices that hold the tongue in place. Additionally, neuromuscular electrical stimulation (NMES) devices are available; they deliver mild electrical stimulation to the muscles of the tongue and upper airway to keep them toned and prevent the airway from collapsing during sleep.
- Benefits for the User: Oral devices are particularly favoured for their portability, discreetness, and non-invasiveness. Users often experience a significant improvement in sleep quality due to reduced airway obstruction. Moreover, NMES devices may offer a novel approach for those seeking a more advanced treatment that actively engages and strengthens the muscles involved in breathing.
5. Orofacial Therapy
- How it Works: This therapy involves a series of exercises that strengthen and retrain the muscles around the mouth, face, and throat. By focusing on the tongue, lips, and facial muscles, it helps in improving muscle tone and reducing the collapsibility of the upper airway during sleep.
- Benefits for the User:
- Patients of all ages can benefit from orofacial therapy, especially children, as it can be seen as a preventive measure to ensure proper muscle function. It reinforces the structural support of the airways, potentially reducing the severity of sleep apnea symptoms.
- Additionally, it serves as a complementary treatment that can enhance the effectiveness of other sleep apnea interventions. Users often report not only better sleep but also improvements in speech and swallowing functions.
Sleep Apnea Surgical Treatments

Surgical sleep apnea treatments can tackle the root of your sleep apnea effectively. For severe cases of sleep apnea, they might be your best bet. If they seem intimidating – don’t worry, they’re really not. Our doctors at Nuffield will be able to walk you through the individual surgeries.
1. Radiofrequency Ablation (RFA)
Utilises radiofrequency energy to heat and shrink tissues in the throat or tongue base. This process reduces tissue size and stiffness, improving airflow and reducing snoring and symptoms of mild to moderate sleep apnea by preventing airway obstruction.
2. Laser-Assisted Uvulopalatoplasty (LAUP)
LAUP takes a focused approach by using a laser to skillfully remove excess tissue from the uvula and soft palate, clearing the way for unobstructed breathing during sleep. The procedure is straightforward and typically done under local anaesthesia, meaning you’ll be in and out of the clinic without the need for a prolonged hospital stay. It’s particularly effective for reducing snoring and treating mild forms of obstructive sleep apnea.
3. Uvulopalatopharyngoplasty (UPPP)
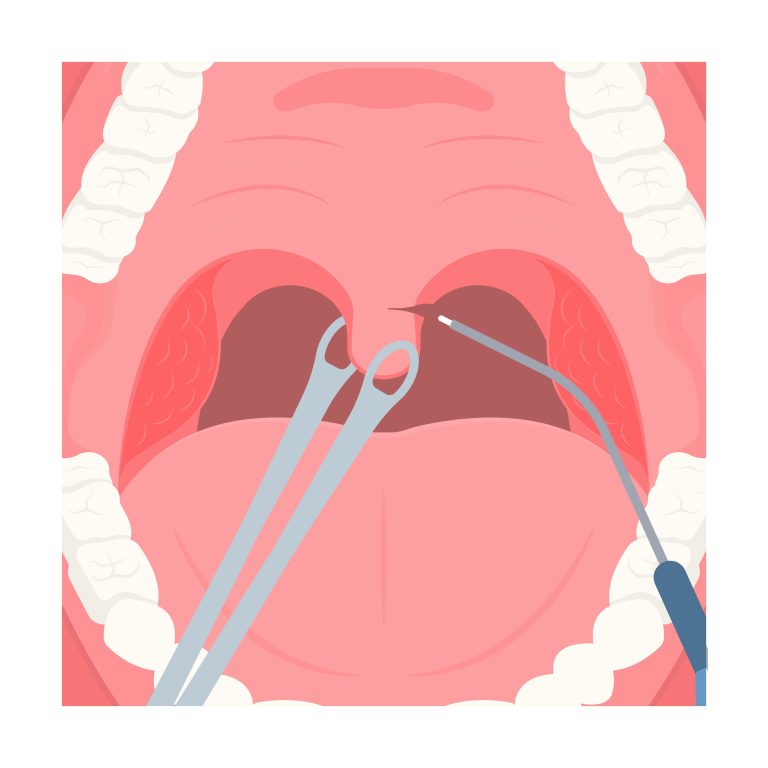
Removes excess tissue in the throat, widening the airway to reduce snoring and treat obstructive sleep apnea. It typically involves removing the tonsils, uvula, and parts of the soft palate. UPPP is more extensive compared to LAUP, but is also more invasive.
4. Tissue Shrinkage
Another option includes tissue shrinkage, where the tissue at the rear of the mouth and the back of the throat is reduced using radiofrequency ablation, a technique suitable for mild to moderate sleep apnea. This method, akin to tissue removal, offers similar effects but with fewer surgical risks.
5. Tracheostomy
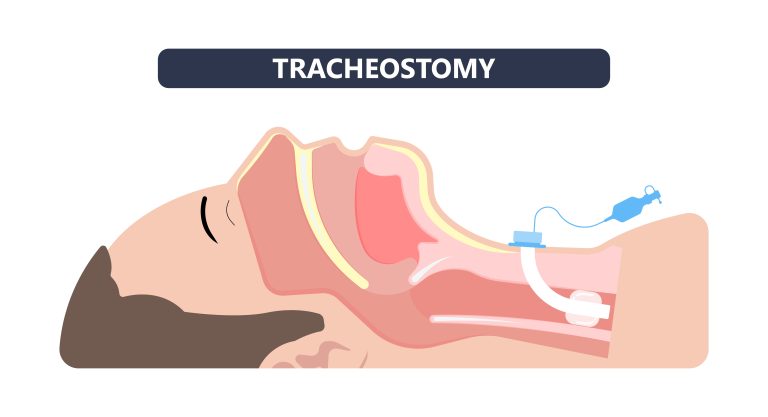
In severe, life-threatening cases of sleep apnea, particularly when other treatments have failed, tracheostomy might be considered. This procedure involves creating an opening in the neck and inserting a tube through which you breathe, establishing a new air passageway. This method is typically reserved for the most extreme cases due to its invasiveness and the lifestyle changes it entails.
6. Maxillomandibular Advancement (MMA)
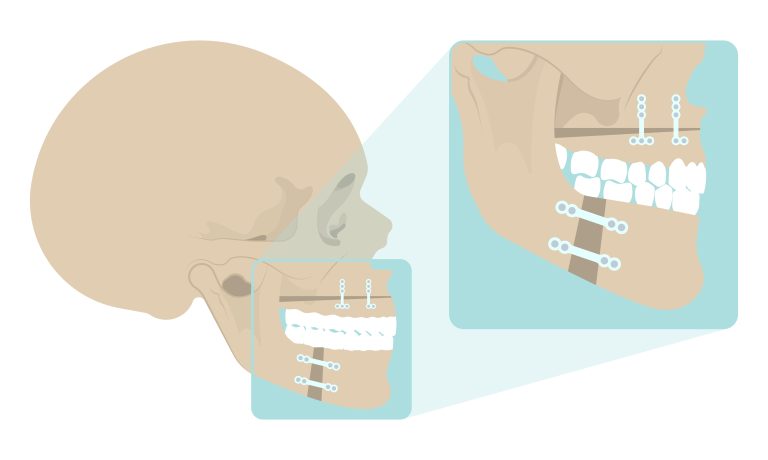
Repositions the upper and lower jaws forward, enlarging the space for breathing in the throat, significantly reducing sleep apnea symptoms by preventing airway collapse.
7. Tonsillectomy and Adenotonsillectomy (T&A)
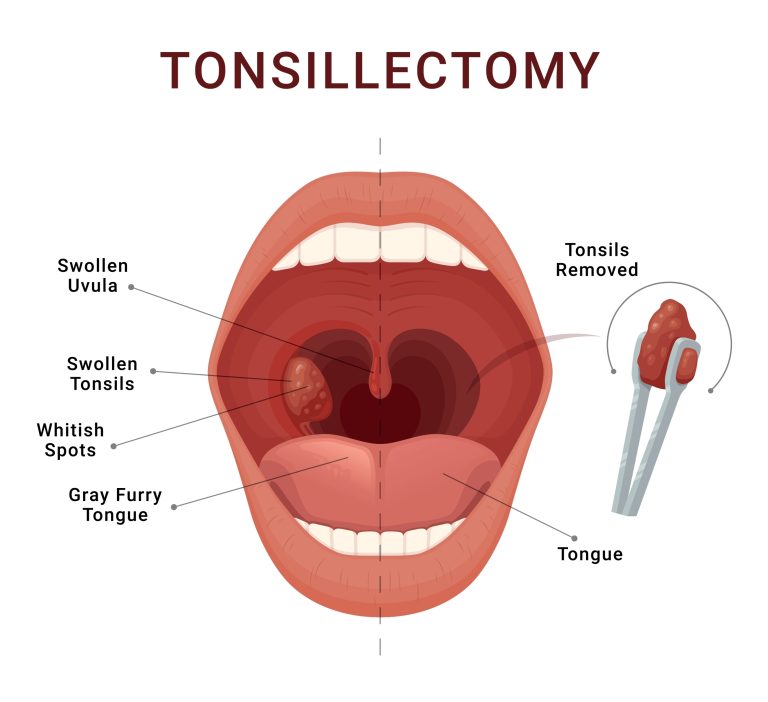
An illustration of how tonsillectomy works.
Involves removing the tonsils (tonsillectomy) and often the adenoids (adenotonsillectomy), clearing the airway to alleviate breathing problems, commonly used to treat sleep apnea in children. As both procedures typically take place within the same surgery session, they’re collectively known as “T&A”.
8. Somnoplasty
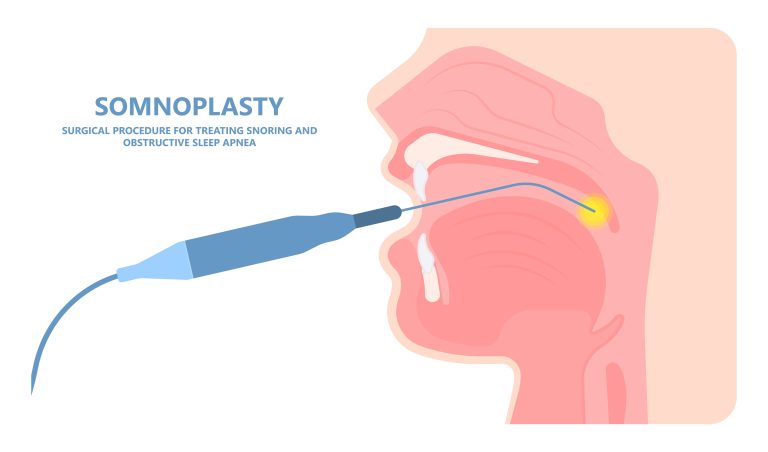
A minimally invasive procedure using radiofrequency energy to reduce and stiffen soft tissue in the upper airway, thereby decreasing snoring and mild obstructive sleep apnea by preventing tissue vibration and collapse.
9. Nasal Surgery
Corrects structural issues in the nose, like deviated septum, to improve airflow, reduce nasal obstruction, and help in treating snoring and obstructive sleep apnea.
10. Pillar Implants (Soft-Palate Implant Surgery)
Involves inserting small, rod-like implants into the soft palate, stiffening it. This procedure reduces the palate’s vibration (a major cause of snoring) and prevents collapse of the upper airway, thereby helping to alleviate snoring and mild sleep apnea.
Treatment for Specific Demographics
Paediatric Sleep Apnea Treatment
Adenotonsillectomy remains the most common treatment for children, but CPAP therapy and weight management are also effective.
Elderly Patients
Tailored CPAP therapy, dental appliances, and positional therapy are considered, along with a comprehensive review of any underlying conditions.

Sleep Apnea Treatment: From Diagnosis to Recovery
While no universal ‘cure’ exists for sleep apnea, a range of treatments can effectively manage symptoms. The journey from diagnosis to recovery involves understanding the process and making informed choices
Diagnosis
1. Recognise Symptoms: Snoring, daytime fatigue, and interrupted breathing.
2. Consult a Doctor: Discuss symptoms and undergo a review of your medical history. To identify the sites of obstruction, the doctor may use nasendoscopy (a medical examination where a thin, flexible tube with a camera is used) to examine the following parts of your face:
- Tonsils
- Soft Palate
- Lateral Pharyngeal Walls (side of throat)
Nose - Epiglottis
- Adenoid Tissue (back of the nose)
- Tongue Base
- Sleep Study: Undertake polysomnography, available in-lab or at-home, to monitor breathing, oxygen levels, and sleep stages.
- Tip: Maintain a sleep diary detailing sleep patterns and daytime feelings.
Treatment
1. Understand Options: Discuss with your doctor the treatment options including lifestyle changes, CPAP therapy, oral appliances, or surgery.
2. Implement Lifestyle Changes: Make manageable adjustments like weight loss, avoiding alcohol before bedtime, and altering sleep positions. Here are the factors within your control.
- Weight Management: Achieving and maintaining a healthy weight can reduce the severity of sleep apnea and frequency of episodes. In particular, effective management of OSA often includes a focus on weight loss, as excess fat deposited in the tongue, muscles, and soft tissues of the upper airway can significantly increase the risk of airway collapse during sleep.
- Regular Physical Activity: Engaging in regular exercise can improve sleep quality and reduce symptoms.
- Proper Sleep Hygiene: Establishing a regular sleep schedule and ensuring a comfortable sleep environment can enhance the effectiveness of other treatments.
- Diet and Substance Moderation: Limiting the intake of alcohol, caffeine, and quitting smoking are crucial steps in managing sleep apnea.
3. Start Therapy or Surgery: Get fitted for a CPAP mask or discuss surgical procedures and their outcomes.
- Tip: Be patient with mask adjustments and communicate with your healthcare provider for any concerns.
A specific treatment would be recommended to you based on the initial diagnosis results. A list of treatments can be found below.
A specific treatment would be recommended to you based on the initial diagnosis results. A list of treatments can be found below.
Non-invasive Treatments
- CPAP (Continuous Positive Airway Pressure) Machines
- BiPAP (Bilevel Positive Airway Pressure) Machines
- Adaptive Servo-Ventilation (ASV)
- Oral Devices
- Orofacial Therapy
Surgical Treatments
- Radiofrequency Ablation (RFA)
- Laser-Assisted Uvulopalatoplasty (LAUP)
- Uvulopalatopharyngoplasty (UPPP)
- Tissue Shrinkage
- Tracheostomy
- Maxillomandibular Advancement (MMA)
- Tonsillectomy and Adenotonsillectomy (T&A)
- Somnoplasty
- Nasal Surgery
- Pillar Implants (Soft-Palate Implant Surgery)
Recovery
- Follow Guidelines: Adhere to post-treatment or post-surgery plans including dietary changes and activity limitations.
- Regular Check-Ups: Monitor progress and adjust treatments as necessary.
- Monitor Changes: Track sleep quality and symptoms, reporting any concerns to your doctor.
- Ongoing Management: Maintain a healthy lifestyle including sleep hygiene and regular exercise.
- Tip: Ensure regular maintenance of CPAP equipment and be open to treatment adjustments if needed.
Tip: Document your journey in a journal as a reference for discussions with your healthcare provider and consider joining support groups for additional guidance.
Benefits of Sleep Apnea Treatment in Singapore

Addressing sleep apnea is not just about silencing snoring; it’s about embracing a healthier, more vibrant life. In Singapore, where modern healthcare merges with cutting-edge technology, sleep apnea treatment brings a plethora of benefits:
- Improved Sleep Quality: Treatment transforms nights of interrupted breathing into continuous, restful sleep, directly enhancing life quality.
- Cardiovascular Health: By managing sleep apnea, you significantly reduce the risks associated with heart disease, stroke, and even diabetes, effectively safeguarding your heart health.
- Elevated Daytime Vigor: Say goodbye to daytime fatigue. Effective treatment ensures you wake up rejuvenated, ready to tackle the day with renewed energy.
- Stabilised Blood Pressure: Regular treatment can lead to lower blood pressure levels, contributing to overall cardiovascular wellness.
- Sharper Focus and Enhanced Mood: With uninterrupted sleep, your concentration sharpens, and mood improves, fostering positive interactions and productivity.
- Safety on the Road and at Work: Proper treatment significantly decreases the likelihood of accidents in your daily commute or workplace, ensuring your safety and that of others.
Sleep Apnea Treatment Risks in Singapore
While treatment offers transformative benefits, it’s also crucial to be aware of potential risks, ensuring you make informed healthcare decisions:
- CPAP Challenges: Some individuals experience discomfort or nasal congestion with CPAP machines. However, advancements in technology and tailored mask fittings can mitigate these issues.
- Surgical Considerations: Surgical interventions for sleep apnea, though effective, come with inherent risks such as bleeding, infection, or extended recovery times. A thorough consultation with your specialist in Singapore can help weigh these risks against the benefits.
Oral Appliance Adjustments: While oral appliances are less invasive options, they might lead to jaw pain or dental shifting over time. Regular dental check-ups and consultations with your sleep specialist are key to managing these potential issues effectively.
Estimated Costs of Sleep Apnea Treatment in Singapore
Please bear in mind that the figures provided are estimates. Actual costs can vary based on individual circumstances, the specific healthcare provider, and any additional treatments or services that may be required.
Diagnostic Costs
| Cost Item | Estimated Costs (SGD) |
| Initial Consultation | $150 |
| Diagnostics Flexible Nasendoscopy Sleep Study | $250 $500 |
| Total Diagnostic Costs | $900 |
Are There Subsidies for Sleep Apnea Treatment in Singapore?
Cost-Saving Opportunities (Considerations):
- Insurance and Medisave: In Singapore, insurance coverage for sleep apnea treatment can vary. Consultation, nasal scopes, and medications are generally covered by insurance and Medisave. However, coverage for sleep studies, CPAP machines, and surgical interventions can be more complex and may vary between different insurers. Patients are advised to check their specific coverage entitlements beforehand.
- Hospital Financial Counselling Services: Most hospitals and clinics in Singapore offer financial counselling services to help patients understand the costs involved and their payment options, including the use of Medisave and insurance.
Why Should I Choose Nuffield for Sleep Apnea Treatment?
Choose Nuffield for sleep apnea treatment for unparalleled expertise and tailored care. Our experienced, credentialed specialists are dedicated to sleep disorders, employing diagnostics and treatment facilities. We offer tailored treatment plans, ensuring you receive comprehensive care, including diligent follow-up and maintenance support. Trust Nuffield to be your partner in navigating sleep apnea treatment effectively. Contact us for a quote today!
Nuffield's Sleep Specialists


Dr. Rebecca Heywood: Dr. Rebecca Heywood, a distinguished British ENT surgeon, brings over 25 years of medical expertise, specialising in otology and hearing implants. Graduating from the University of Manchester and training at globally recognized institutions, she’s acclaimed for her patient-centred care, receiving a Gold Singapore Health Quality Service Award in 2022. With international exposure, including the House Ear Institute and Ear Science Institute Australia, she’s recognized for pioneering hearing implant programs in Singapore, demonstrating her leadership and commitment to enhancing patient hearing experiences.
Dr. Vyas Prasad: Dr. Vyas Prasad, an esteemed Otolaryngologist-Head and Neck Surgeon, trained at Trinity College, Dublin, and in top UK programs, brings a rich background in surgery and ENT. Recognized for his contributions to bariatric surgery with a Master’s from Imperial College, his expertise extends to adult and paediatric care, honed in renowned London hospitals. At Ng Teng Fong General Hospital, Singapore, he spearheaded the laryngology service, excelling in voice, swallowing disorders, and minimally invasive head and neck surgery. His holistic approach to sleep apnea care integrates this extensive surgical expertise with a deep understanding of patient needs.
Conclusion
Treating sleep apnea effectively enhances your life, offering restful nights and energised days. It not only boosts sleep quality but also uplifts mood and sharpens the mind. In Singapore’s advanced healthcare landscape, a variety of effective treatments ensure not just quiet nights but also vibrant, active days.
Medical References
Chang, H., Chen, Y., & Du, J. (2019). Obstructive sleep apnea treatment in adults. Kaohsiung Journal of Medical Sciences, 36(1), 7–12. https://doi.org/10.1002/kjm2.12130
Penzel, T., Schöbel, C., & Fietze, I. (2018). New technology to assess sleep apnea: wearables, smartphones, and accessories. F1000Research, 7, 413. https://doi.org/10.12688/f1000research.13010.1
Xu, T., You, D., & Chen, X. (2017). Non-surgical treatment of obstructive sleep apnea syndrome. European Archives of Oto-Rhino-Laryngology, 275(2), 335–346. https://doi.org/10.1007/s00405-017-4818-y
FAQs
1. How Long is a Sleep Apnea Treatment?
The duration of sleep apnea treatment varies based on the method chosen. Non-invasive treatments like CPAP may be ongoing, while surgical options have a defined recovery period. Continuous follow-up is essential for maintaining treatment effectiveness.
2. How Many Sessions of Sleep Apnea Treatment are Recommended?
The number of treatment sessions depends on the type and severity of sleep apnea. Non-invasive treatments are often daily, whereas surgical treatments usually require one procedure followed by several follow-up appointments.
3. Does Sleep Apnea Treatment Hurt?
Non-invasive treatments like CPAP are painless. Surgical options may involve postoperative discomfort, but pain management is part of the recovery process. Your healthcare provider will ensure your comfort and address any pain-related concerns.
4. Is There a Minimum Age for Sleep Apnea Treatment?
No. Treatment methods are tailored to the patient’s age and specific needs, with paediatric sleep apnea treatments available for younger patients.
5. What Should I Avoid After Sleep Apnea Treatment?
Post-treatment guidelines depend on the type of treatment received. For surgical treatments, avoiding strenuous activities and following dietary recommendations are common. Your doctor will provide specific instructions based on your treatment.
6. How Will I Feel After Sleep Apnea Treatment?
Patients often report improved sleep quality and overall health following effective treatment. Initial adjustment periods, especially for CPAP users, are common, but long-term benefits include better sleep and reduced health risks.
7. Is it Worth Going for Sleep Apnea Treatment?
Absolutely. Treating sleep apnea is crucial for preventing long-term health complications like heart disease and improving quality of life. Consult with a healthcare provider to determine the best treatment for your situation.
8. Is Sleep Apnea Treatment Regulated in Singapore?
Yes, sleep apnea treatment in Singapore is regulated and provided by certified healthcare professionals. Treatments adhere to national healthcare standards, ensuring patient safety and efficacy.
9. Are There Home Treatments For Sleep Apnea?
Yes. However, for proper diagnosis and treatment, we highly recommend consulting a healthcare professional. Usage of unverified home treatments may worsen your sleep apnea.
