Obstructive Sleep Apnea (OSA): Exploring the Condition That Affects Nearly 1 in 3 Singaporeans
Research has revealed that 1 in 3 Singaporeans struggle with Obstructive Sleep Apnoea (OSA). It occurs when breathing frequently stops and starts during slumber.
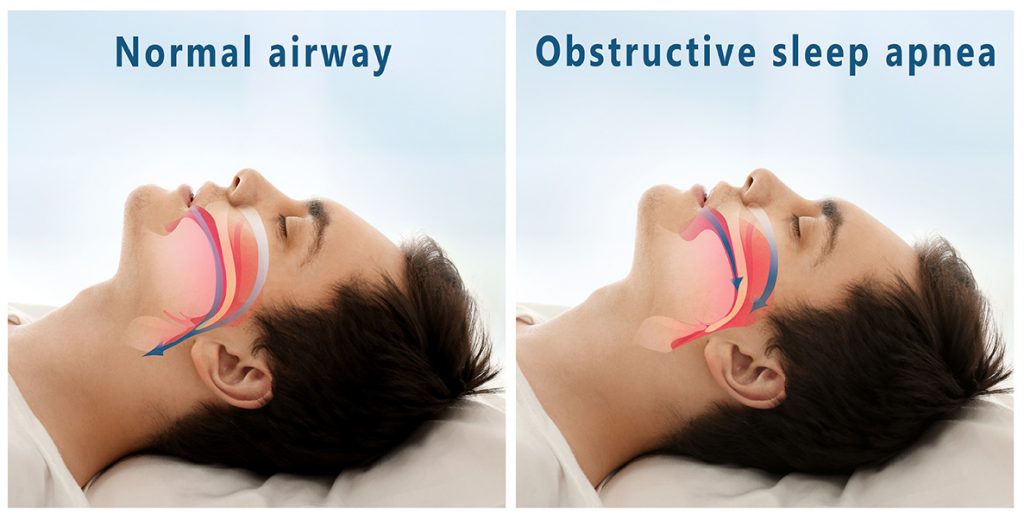
What is Obstructive Sleep Apnea (OSA)?
Obstructive sleep apnea (OSA) is a respiratory condition characterised by temporary pauses in breathing, which arise from significant reductions in airflow through the upper airways during sleep. Airway obstruction can have a serious impact on a person’s overall health and quality of life, putting them at greater risk of contracting diseases such as congestive heart failure and stroke. Let’s take a closer look at obstructive sleep apnea, a disease that’s estimated to affect 1 billion people worldwide. In this article, we’ll cover OSA’s symptoms, causes, and consequences, as well as the methods for diagnosing and treating this sleep-related breathing disorder.
Causes of OSA
Obstructive Sleep Apnea (OSA) arises from various factors that lead to the narrowing or closure of the airway during sleep. Key causes include:
- Anatomical Variations: Individuals with smaller or structurally unique throats may face severe narrowing, blocking significant airflow.
- Obesity: Excess weight contributes to soft tissue accumulation in the throat and neck, further restricting airway space.
- OSA is marked by significant breathing interruptions, namely:
- Hypopnea: A decrease in airflow by at least 30% for 10 seconds or more.
- Apnea: A 90% or greater reduction in airflow for at least 10 seconds.
Diagnosis often involves identifying more than five apneas or hypopneas per hour, especially if observed by others or resulting in health issues. If you’re concerned about yourself or a loved one, contact Nuffield ENT and get assessed by our doctors.

Obstructive Sleep Apnea Risk Factors
The following factors contribute to your risk of getting OSA.
- Excess weight: Soft tissue is accumulated in the throat and tongue, contributing to airway blockage.
- BMI: A higher Body Mass Index (BMI) is closely linked to increased risk of OSA. Overweight and obese individuals, defined as having a BMI of 25 and above, have a higher likelihood of developing OSA due to the reasons associated with excess weight.
- High Blood Pressure: The repeated episodes of low oxygen levels and the stress of waking up frequently can lead to increased blood pressure. Individuals with hypertension are at a higher risk of developing OSA, creating a vicious cycle that exacerbates both conditions.
- Ageing: With age, muscles in the neck circumference of the throat and tongue lose tone, increasing the risk of blockage.
- Gender: Men are more likely than women to develop obstructive sleep apnea, with hormonal differences and fat distribution patterns contributing to the disparity in risk between genders.
- Hypertrophy of soft tissue: Enlargement of adenoids, and tonsils, can serve as obstacles to normal breathing during sleep. Specifically, large tonsils can significantly narrow the airway, especially in children, which is a critical factor contributing to the increased risk of OSA. In such cases, a tonsillectomy may be considered to remove the enlarged tonsils and improve airway patency.
- Structural features of the face and throat: Certain structural characteristics can predispose individuals to OSA. These include:
- Small or Recessed Lower Jaw: A lower jaw that is small or positioned farther back can reduce the airway size, making it more prone to obstruction.
- Enlarged Tongue: An enlarged base of the tongue can obstruct the airway, particularly during sleep when muscle tone decreases.
- Neck Circumference and Excess Throat Fat: A neck size larger than 17 inches in men is a strong predictor of OSA. Excess fat surrounding the throat can further narrow the airway, increasing the likelihood of obstruction.
- Regular intake of alcohol and sedatives: Alcohol and some medications, such as muscle relaxants and antispasmodics, can contribute to airway obstruction.
- Smoking: This harmful habit often causes inflammation and swelling of the mucous membranes, exacerbating obstructive sleep apnea.
- Diseases and allergies: Asthma, rhinitis, sinusitis, as well as allergic reactions, can increase the likelihood of airway obstruction during sleep.
- Ethnicity: In Singapore, Chinese men are more prone to developing obstructive sleep apnea compared to Indian and Malay men.
- Hormonal changes: The risk of developing OSA increases after menopause, a scientifically proven fact.
Types of Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) varies by severity and age group, affecting both children and adults. The distinctions between mild, moderate, and severe OSA, as well as Pediatric OSA, lie in the frequency and impact of symptoms rather than the fundamental nature of the disorder.
Mild Obstructive Sleep Apnea
- Characterised by loud snoring and brief pauses in breathing.
- Symptoms include morning fatigue, daytime sleepiness, severe morning headaches, impaired concentration, and mood changes like irritability and anxiety.
- Increased risk of heart disease and stroke.
Moderate Obstructive Sleep Apnea
- Features more frequent and intense episodes than mild OSA, including loud, persistent snoring and waking up choking or gasping.
- Leads to significant daytime fatigue, increased accident risk, cognitive difficulties, mood disturbances, and a higher risk of hypertension and cardiovascular issues.
- Management often involves CPAP therapy or other airway support, with regular specialist follow-up for treatment adjustment.
Severe Obstructive Sleep Apnea
- Marked by extremely loud snoring, prolonged breathing pauses, and frequent awakenings.
- Symptoms include significant daytime sleepiness, pronounced morning headaches, and a markedly increased risk of cardiovascular diseases and stroke.
- Results in a substantial decrease in sleep quality and overall life quality.
- Requires advanced airway management strategies, including CPAP therapy and potentially surgery.
Pediatric Obstructive Sleep Apnea (Sleep Apnea in Children)
- Management of sleep apnea in children requires consideration of growth and developmental aspects.
- Treatments include tonsillectomy, adenoidectomy, positive airway pressure therapy, and orthodontic interventions.
- Symptoms include loud snoring and episodes of breathing cessation, leading to restless sleep.
- Symptoms that mirror ADHD, such as hyperactivity, difficulty focusing, or poor school performance.
- Other signs are bedwetting, frequent limb movements during sleep, abnormal sleeping positions, or sleeping with an extended neck.
- Possible manifestations include reflux or night sweats.
- Daytime sleepiness, behavioural issues, and learning difficulties impact psychosocial and physical development.
- In severe cases, there may be a potential for growth and developmental delays.
- Treatment is tailored to individual needs, utilising both surgical and non-surgical options to address paediatric OSA symptoms.
Stages of Obstructive Sleep Apnea
The severity of obstructive sleep apnea is based on a score from a scale known as the apnea-hypopnea index (AHI). This index calculates the average number of times you have episodes of apnea and hypopnea for every hour you’re asleep.
Stage of OSA | Diagnostic Criteria |
Mild obstructive sleep apnea | AHI: >30 per hour. |
Moderate obstructive sleep apnea | AHI: 15-30 per hour. |
Severe obstructive sleep apnea | AHI: 5-15 per hour. |
Obstructive Sleep Apnea Symptoms
Recognizing and addressing the symptoms of Obstructive Sleep Apnea (OSA) is essential for reducing its health risks and enhancing quality of life. Symptoms indicative of OSA include:
- Loud snoring, particularly pronounced when lying on the back.
- Instances of breathing pauses observed by others.
- Awakening with a sensation of gasping or choking.
- Restless sleep characterised by frequent awakenings.
- Excessive daytime sleepiness, leading to a high likelihood of napping.
- Cognitive difficulties, such as impaired concentration and memory.
- Night sweating more than usual.
- Morning headaches, often a result of lowered oxygen levels during sleep.
- Mood changes, manifesting as irritability or depression.
Addressing these symptoms promptly can significantly improve health outcomes and mitigate the risks associated with OSA.

Obstructive Sleep Apnea Diagnosis Criteria
OSA is associated with various risks, such as elevated blood pressure, diabetes mellitus, cardiovascular diseases, and even memory issues. Here are some ways in which it is diagnosed.
Medical History
When diagnosing obstructive sleep apnea (OSA), specialists typically look at:
- Sleep patterns. The patient might undergo sleep tests and provide information about their sleep onset time, awakenings, frequency of nighttime awakenings, and morning sensations.
- Symptoms during sleep. Patients are encouraged to describe their symptoms in detail, indicating whether there is loud snoring, moments of choking or feeling of breathlessness, night sweats, increased anxiety, and other relevant factors.
- Daytime symptoms. Doctors inquire about daytime sleepiness, fatigue, decreased concentration, and other factors that may indicate disruptions due to lack of sleep.
- Risk factors. Patients are evaluated for excess weight, hereditary conditions, regular alcohol consumption, smoking, and other relevant factors.
Physical Exam
The physical examination of a patient with obstructive sleep apnea includes an assessment of the anatomy of the throat, weight, neck circumference, and oral and throat cavity. The doctor also measures blood pressure, inspects the skin for oxygen saturation, and checks reflexes. These measures, along with home sleep apnea testing, help identify signs and factors associated with OSA, determine the stage of the condition, and facilitate the selection of the most effective treatment.
Sleep Study
Specialists need to conduct a detailed sleep study in patients with apnea, starting with collecting a history of sleep quality. They study obstructive sleep apnea diagnosis criteria and ask questions about sleep patterns, duration, and nighttime awakenings.
Doctors may also use oxygen and breathing monitoring to detect apnea episodes and assess blood oxygen levels, which are crucial for understanding the health implications of OSA. Reduced oxygen levels during sleep can lead to various health issues, including cardiovascular diseases, cognitive impairment, and metabolic disorders.
STOP-BANG Questionnaire
The STOP-Bang Questionnaire serves as a practical tool for clinicians to screen for potential obstructive sleep apnea (OSA) in individuals. It includes eight dichotomous queries that reflect the primary risk elements for OSA. The acronym STOP-Bang encapsulates key indicators or characteristics often linked with the disorder:
- “Snoring” asks if one’s snoring is significant enough to disturb a sleeping partner.
- “Tiredness” captures the experience of daytime fatigue, including instances of dozing off during routine activities.
- “Observed Apnea” relates to incidences where a person has been seen to cease breathing momentarily while sleeping.
- “Pressure” correlates to the presence of hypertension.
- “BMI” considers whether the body mass index exceeds 35, a known risk factor.
- “Age” targets the risk increase in individuals over the age of 50.
- “Neck Circumference” measures the neck, where a circumference above 16 inches may suggest higher risk.
- “Gender” notes that males are generally at a higher risk of developing OSA.
This assessment is designed to streamline the preliminary identification process for OSA in a clinical setting.
Home Sleep Apnea Testing
Home Sleep Apnea Testing is a method of diagnosing sleep apnea conducted in home settings. Patients are provided with portable devices for sleep monitoring, which measure brain activity, breathing, pulse, oxygen levels, and body position. These devices offer a more comfortable and natural environment for falling asleep than polysomnography in specialised laboratories. Doctors analyse the data collected to detect the presence of apnea and determine its characteristics.
Nuffield ENT is always ready to help. If you’re struggling with the lack of sleep, schedule a consultation with our friendly team.
Obstructive Sleep Apnea Treatment Options
CPAP
Continuous Positive Airway Pressure (CPAP) is a standard severe obstructive sleep apnea treatment. The device consists of a pump connected to a mask that fits snugly over the patient’s nose or nose and mouth. During sleep, CPAP maintains constant pressure in the upper airway, preventing tissue collapse and ensuring unobstructed breathing. CPAP not only reduces loud snoring and morning fatigue but also lowers the risk of cardiovascular complications associated with apnea.
BiPAP
Bilevel Positive Airway Pressure (BiPAP) represents an advanced form of respiratory therapy. The device also consists of a pump and mask, but unlike CPAP, BiPAP provides two pressure levels for inhalation and exhalation. This allows patients to breathe more comfortably, especially beneficial for those experiencing difficulty exhaling. BiPAP is widely used for severe cases of apnea and in patients with other respiratory disorders. This therapy method can be adjusted according to the patient’s needs, providing a more personalised approach to treatment.
APAP
Automatic Positive Airway Pressure (APAP) is a modern treatment method for sleep apnea, combining the advantages of CPAP and BiPAP. The device automatically adjusts the pressure level in the airway based on the patient’s needs, dynamically adapting it during sleep. It more accurately maintains airway patency, particularly useful during changes in body position or sleep stages. APAP is more comfortable for the patient, providing effective apnea treatment and minimising potential side effects.
Surgery
If conservative treatment is of little help or not helpful, doctors offer surgical intervention to patients. Let’s consider each type of surgical treatment for the pathology in more detail and highlight its essential characteristics.
Nasal Surgery
This often involves correcting septal deformities, reducing the size of nasal turbinates, and removing polyps to improve airway patency. The intervention aims to eliminate obstacles that may obstruct the upper airways, especially in the nasal area.
Palatal Surgery
Typically, it involves removing tonsils and adenoids, especially in children, to improve breathing. This procedure, known as tonsillectomy and adenoidectomy, reduces the likelihood of airway blockage during sleep and decreases apnea frequency.
Hypopharyngeal Surgery
The essence of the intervention is to remove obstacles in the back of the throat and pharynx. This may include strengthening or reconstructing tissues.
Tracheostomy
Involves creating an opening in the trachea directly below the throat to provide direct access to air. It is used for severe cases of apnea when other treatment methods are ineffective. Tracheostomy ensures unobstructed airflow, bypassing the upper airways, and may be a temporary or permanent solution depending on the severity of the case and other indications.
Maxillomandibular Advancement Surgery
This surgical manipulation, known as genioglossoplasty, aims to improve the space in the back of the throat. It involves redistributing or increasing the volume of soft tissues, reducing the likelihood of apnea recurrence.
Central Sleep Apnea vs Obstructive Sleep Apnea
Central Sleep Apnea (CSA) and Obstructive Sleep Apnea (OSA) are distinct disorders, differing mainly in their causes and mechanisms, yet both significantly impact sleep quality and overall health. Here’s how you can differentiate between the two.
| Оbstructive sleep apnea diagnosis criteria | Central Sleep Apnea | Obstructive Sleep Apnea |
| Cause | Closure of the upper airways | Absence of brain signal for breathing |
| Mechanism | Physical obstruction of airways | Disruption of central respiratory control |
| Snoring | Characterised, often by pronounced snoring | Usually absent or mild |
| Diagnosis | Polysomnography (PSG) examination | Polysomnography (PSG) detecting central apneas |
| Treatment | Typically involves CPAP and surgical methods | Often requires BiPAP or adaptive devices, treating the underlying cause |
| Prognosis | Complications such as arterial hypertension, stroke are possible | Associated with more serious conditions and necessitates individualised treatment approach |
OSA Risks
High blood pressure
Heart disease
Heart attack

Stroke
Type 2 diabetes
- OSA increases the likelihood of hypertension, cardiovascular disease, and type 2 diabetes.
- Leads to weight gain through hormonal imbalances affecting appetite.
- Raises the risk of workplace or driving accidents due to impaired concentration and excessive daytime sleepiness.
OSA Complications
- Untreated OSA can lead to stroke, heart failure, and irregular heartbeats.
- May worsen existing cardiovascular conditions, negatively affecting heart health.
- Can contribute to mental health issues like depression and anxiety.
- Impacts cognitive functions, potentially causing memory loss and decreased alertness.
FAQ
1. Is Obstructive Sleep Apnea a Disability?
Yes, the condition may be recognised as a disability if it significantly restricts everyday activities and work capacity.
2. Is Obstructive Sleep Apnea Genetic?
Genetics can influence the anatomical features of the upper airways, increasing the risk of developing OSA.
3. What Impact Does OSA Have on my Daily Activities?
The condition can lead to daytime sleepiness, fatigue, reduced concentration, and efficiency. Memory and mood problems may also arise.
4. Can Obstructive Sleep Apnea be Cured?
No, while not always curable, treatments like CPAP devices, surgery, or lifestyle modifications can manage symptoms effectively.
5. What Happens if OSA Were to Go Untreated?
If left untreated, obstructive sleep apnea could lead to serious health problems, including cardiovascular diseases, high blood pressure, or stroke.
6. How Can I Support a Loved One with Obstructive Sleep Apnea?
Encourage your loved one to adhere to medical advice, help them to set up a calm sleeping environment, and promote healthy lifestyle choices.
7. Do I Need to See an ENT Specialist for Obstructive Sleep Apnea?
Yes. ENT specialists are skilled in treating airway issues, making them invaluable for diagnosing and managing OSA.
8. When Should I Call My Healthcare Provider?
Seek medical help if you experience loud snoring, prolonged pauses in breathing during sleep, or daytime sleepiness.
Medical References
Gottlieb, D. J., & Punjabi, N. M. (2020). Diagnosis and management of obstructive sleep apnea. JAMA, 323(14), 1389. https://doi.org/10.1001/jama.2020.3514
Lim, D. C., & Pack, A. I. (2017). Obstructive sleep apnea: update and future. Annual Review of Medicine, 68(1), 99–112. https://doi.org/10.1146/annurev-med-042915-102623
Osman, A. A., Carter, S. G., & Carberry, J. C. (2018). Obstructive sleep apnea: current perspectives. Nature and Science of Sleep, Volume 10, 21–34. https://doi.org/10.2147/nss.s124657
Patil, S. P., Schneider, H., Schwartz, A. R., & Smith, P. L. (2007). Adult Obstructive sleep apnea. Chest, 132(1), 325–337. https://doi.org/10.1378/chest.07-0040
Schröder, C., & O’Hara, R. (2005). Depression and Obstructive sleep apnea (OSA). Annals of General Psychiatry, 4(1). https://doi.org/10.1186/1744-859x-4-13
